I cannot believe I didn’t blog the entire month of April. I knew it had been a while, but I didn’t think it had been that long. I sat down this morning to do some writing and look over the blog design, as well as my Thoughts and Ramblings Facebook page, and I realized how much I have missed writing. I also realized that last month was the FIVE year anniversary of this blog!
Lots of stuff has been going on. For the past couple of months I have been working vigorously on a few things to help improve my quality of life, physically, mentally, and spiritually. I will be honest, it has been super tough. It usually is when you take an honest look at who you are, where you came from, and where you want to be headed. It has meant being rigorously honest with myself and well, let’s face it, that can really suck sometimes. However, I am now seeing the benefits of all that hard work and I am excited about the future.
It can also be tough heading into uncharted territory in regards to my health. I have had some neuropathy issues going on as well as some possible autonomic neuropathy issues. I am currently on an aggressive alternative medicine course to try and manage those symptoms and if that doesn’t work, I already have a very precise and well thought out traditional medicine plan worked out with my rheumatologist in terms of testing and figuring this all out. My guess is, it will be a combination of both alternative and traditional medicine that will help me deal with this new part of my Sjögren’s journey.
The good news is that I realized yesterday that for the first time since the autoimmune journey began around 2007/2008, this is the most confident I have ever felt with every single one of my medical providers. I have had some great doctors in the past, but at this point I feel like I am being completely heard and I am an active partner with every one of my medical providers. I have ten providers (both alternative and traditional) that I am actively seeing now and I don’t experience the anxiety I used to have. As I have talked about before, I made some difficult decisions last year about switching some of my providers in order to obtain better care and it’s nice to see that those decisions worked out for the best.
Besides the neuropathy pain and dryness issues, I am actually holding my own. My joint pain and fatigue have improved dramatically. I am certain that the improvement in the fatigue is related to someone FINALLY listening to me and following through about my thyroid and making some medication adjustments, as well as a change in my nutrition. The thyroid is not perfectly regulated, but it is much improved. Everybody kept blaming the fatigue solely on the Sjögren’s when I have also had this longstanding thyroid issue since I had radiation to my neck a million years ago.
Besides working at my nursing job more recently, one of the other reasons I have been off the blog grid is that I have been working hard at changing the way I deal with Sjögren’s and my health. That has been a gradual process for a few years, but I have been looking at it much differently lately. I think I have blogged before that I see a therapist who has experience in dealing with chronic illnesses and we have definitely made progress.
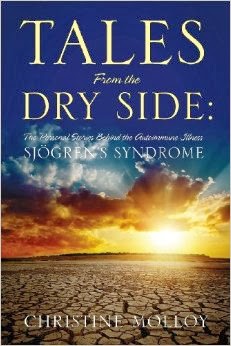
However, things kind of got to the point a few months ago where I was just sick and tired of talking about this illness all the time. I wrote a book about it, I talk about it at appointments all the time, and I was blogging about it a lot. Thoughts and Ramblings, and its associated Facebook page, is not all about Sjögren’s or even autoimmune disease, but that’s the direction it happens to take because so many of my readers have autoimmune illnesses and it is a place to share and exchange good information about the illnesses and their treatments.
And that’s not going to change; but I was at a point where I needed a divorce from Sjögren’s for a while. We all know that it’s more like a separation rather than a divorce, and even the separation can only be partial because this illness invades every aspect of our lives. But I was able to find some separation. I stopped complaining about all my symptoms either on social media or to my family/friends. I stopped doing follow-up appointments with doctors just for the sake of having a follow-up appointment when things had been stable in that particular area. I stopped researching stuff online and lessened my visit frequency to the online Sjögren’s groups. I still took my medications and attended necessary appointments. I was still spending about two hours a day dealing with the illness and its symptoms. But two hours a day was better than four!
I decided that for now, I am not writing another Sjögren’s book.
I felt guilty at first because I know this blog, the Facebook page, and me as an individual have a lot to offer to those suffering from autoimmune illnesses. And, they (and I) will still be here. But my brain cannot be Sjögren’s focused all the time for the rest of my life. I found that when I did do this separation, it was a very good thing. I pushed myself harder, especially at work and other projects, and I found that I can be of use to this world in other ways. I also found that my anxiety lessened significantly, I wasn’t as fearful, and I could cope better with the physical challenges that did come my way.
I have been criticized in the past (even by a person with Sjögren’s), and somewhat recently, for some of the things I say and especially write, in regards to keeping a positive outlook when dealing with a chronic illness. The feedback mentioned that I may not always be realistic in how miserable this illness can be and that not every autoimmune story has a happy ending or a positive lesson to teach. Or I’m told I must have a mild case of Sjögren’s because I am upbeat. I tell them to go read my blog for the past five years and read about my journey. My attitude and disposition is inversely proportional to my physical experiences. I have a positive attitude most days, not because I don’t suffer or struggle, but because I actually get to be alive.
And loved.
And I get to love back.
I know many people may not want to hear this, but I think many times, myself included, we get ourselves so wrapped up in our illness that we don’t see any other possibilities except to be miserable or be a victim. And you know what? I get to do that sometimes. I get to be upset. But the problem is we take on our illness as our identity instead of it letting it be a part of who we are just like being a nurse or a writer is part of who I am. Rather than living my life as a victim, I want to live it as just me. Chris.Those of us with Sjögren’s do not corner the market on pain and suffering. Those of us with autoimmune diseases do not have exclusive rights to the pain and suffering in the world. We all have something, whether it is physical, emotional, or spiritual pain. It has been that realization that has enabled me to recently step out of Sjögren’s and step into helping someone else. It has enabled me to step out of Sjögren’s and step more into the world.
So what can you step into today?