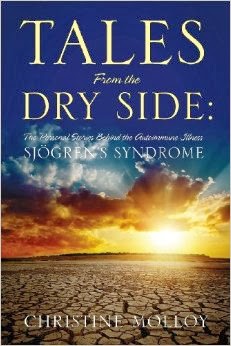
In the two and a half years I have been writing this blog, I don’t think I have ever written a post about a doctor’s appointment with my rheumatologist. The appointments tend to be pretty significant since the rheumatologist treats the Sjogren’s syndrome. I am sure that I have mentioned events that have happened at certain appointments, but I think that has been the extent of it. I think the reason for this is because I don’t think people will be interested or that the post may be boring. Today I realized that I may have made a mistake. Sharing information from these appointments with my rheumatologist not only may help someone else, but it also gives other people the opportunity to give me feedback about their experiences with different treatments, side effects, and complications from medications.
I have had more severe symptoms than usual lately with some new ones thrown in for fun. Therefore I have been seeing my rheumatologist, Dr. P, more often than usual. These appointments tend to be stressful for me compared to those with other doctors. Sjogren’s syndrome, like many other autoimmune diseases, often presents with a myriad of symptoms and often it is like trying to fit together the pieces of a puzzle. Is this symptom autoimmune related? Is it a side effect from a medication? There is the unpredictability of not knowing what the next step may be in treating the illness. Then there is also the fact that Dr. P’s office is an hour away from home, she is usually running behind (I have attributed this to the fact that she does not rush through her visits), and sometimes there is lab work to be done after the visit. From the time I leave my home to the time I pull back in the driveway, I am looking at a five hour trip. Exhausting.
I have been more frustrated than usual with her, myself, and the whole Sjogren’s situation in general. I had just recovered from the whole Guillain-Barre/blood clots in the lungs fiasco when I began to develop severe, debilitating migraines thought to possibly be autoimmune related. After struggling to find a medication at a dose I could tolerate to manage these migraines, some of my Sjogren’s symptoms decided to come out and play; most likely because I had weaned off my steroids. Severe fatigue and joint pain worse than I have had in at least a year were the highlights. In addition to that, I have been having some significant urinary issues that come and go and that has prompted some further testing; the cause thought to possibly be autoimmune or medication related.
What this has meant is that Dr. P and I have been continuously trying to figure out a course of treatment to manage my illness. A course of treatment for an illness that has no cure and really no acceptable or standard form of treatment. If you have diabetes, you change your lifestyle, check your blood sugars, and take insulin. The end result is that most of the time, your illness can be controlled. Not the case with Sjogren’s, or many other autoimmune illnesses for that matter.
And there are only so many medications to try. Appointment after appointment Dr. P and I discuss the options and what may come next in regards to medications. She keeps wanting to put me on or increase my dose of prednisone. This gets me pretty worked up to say the least. If you have spent any time reading my blog, you will understand how much I hate prednisone. Here’s the thing though: as Dr. P said today, I am between a rock and a hard place and it is a matter of choosing the lesser of all evils. I have already been on many of the other autoimmune medications such as methotrexate, Imuran, Cellcept, and Enbrel. Cellcept did help quite a bit but made me so sick that my previous doctor had no choice but to take me off of it. Enbrel helped a little but not enough to justify the chronic sinus infections it was causing me to have.
As we discussed today, there are some other options to consider such as the medications Arava and Rituximab. But they are not without their risks as well. It is hard to make decisions, I am sure for her as well as for me, about which risks to take. Do we consider Imuran again and take the risk of liver damage and other complications or continue trying the steroids at different doses and see what side effects I can live with and risk long term complications such as diabetes, cataracts, and stroke? As much as I hate the prednisone, there is no doubt, it works for most of my symptoms. The problem is that I need a lot of it and the more I take, the worse the side effects are and the higher the risk of severe long term complications.
So our plan for now is to double up my prednisone dose to 15 mg for a few days and then slowly wean it down to 10 mg rather than the 7.5 mg I am currently on. We did this about two weeks ago when the pain and swelling got bad enough to interfere with my daily functioning and it worked but once I got back to 7.5 mg for a few days, the symptoms started up again. So this time we will only wean down to 10 mg. We agreed that 10 mg is the maximum dose of prednisone that is comfortable for me long term. Well, for Dr. P anyways. 0 mg is the maximum dose I am comfortable with but the reality is that my options are getting fewer and fewer and I cannot risk further Sjogren’s complications or live in this state of health.
What I came to understand from my appointment today is that there are no easy answers. Not even easy answers, but any concrete answers.
There is no medication in this world right now that is going to fix me without making me sick in some other way. Maybe someday there will be. But not today.
I am also starting to understand that I don’t think my body is ever going to go back to the point it was at before December 2008, which is when Sjogren’s started to truly ravage my body.
This does not mean that I still cannot do what I am doing; exercising, eating healthier, reducing stress. I will keep trying to control my symptoms through diet and exercise. I will live a healthy lifestyle. I will meditate. I will work with my doctors and stick with my treatment plan. I will laugh and I will play. But I guess for now at least, I am not going to place any of my hopes on any one medication to be the answer for restoring my body to the state that it was once in. Rather, I will continue to work with the body that God has given me in this moment and in this day to live in the best possible way that I can.
Photo Courtesy of Google Images