During my last rheumatology visit, telemedicine style of course, my doctor and I talked about what options are left for me in terms of treating Sjogren’s. By the way, we officially call it Sjogren’s now, and NOT Sjogren’s Syndrome. I can get into that at another time.
I’ve been at this for twelve years now and have gone through a gamut of medication trials. The biggest issue is that there is no cure, or even a targeted treatment, for Sjogren’s. Our rheumatologists do the best they can with medications used for multiple other autoimmune diseases, but we desperately need a treatment targeted for our disease. We, as patients, do the best we can with symptom management, diet, exercise, alternative medicine, and self care.
The whole medication treatment issue for Sjogren’s is much too long to get into in this post, but let’s just say, it’s a crapshoot at best. For me personally, I take a medication called Plaquenil (also known as hydroxychloroquine…you have all heard of that one!) and Evoxac. The Plaquenil is supposed to help my symptoms. I’m not sure how much it does, but I have tried weaning off it without much success and on top of that, it is supposed to help slow down disease progression and that is very important. Evoxac is a medication I take several times a day to stimulate saliva flow because Sjogren’s attacks the saliva glands and there are numerous complications associated with that, most of which I have had at one time or another. I have lost a lot of function in my salivary glands.
Besides those two medications, I rely on prednisone, which is a steroid, when I absolutely have to. Long term prednisone is dangerous and since I require high doses of it, it’s not a sustainable long-term solution. Typically, I go on a course of it one to three times a year. I did make it a year and a half without it once.
At my last visit, we decided that I should go on a round of prednisone. It was a little nerve wracking because of the COVID situation, but the numbers in my state were down and I felt like it was the best time to try and quiet things down, especially because my level of functioning had decreased significantly since Fall 2019 and we don’t know what this Fall will bring in regards to COVID.
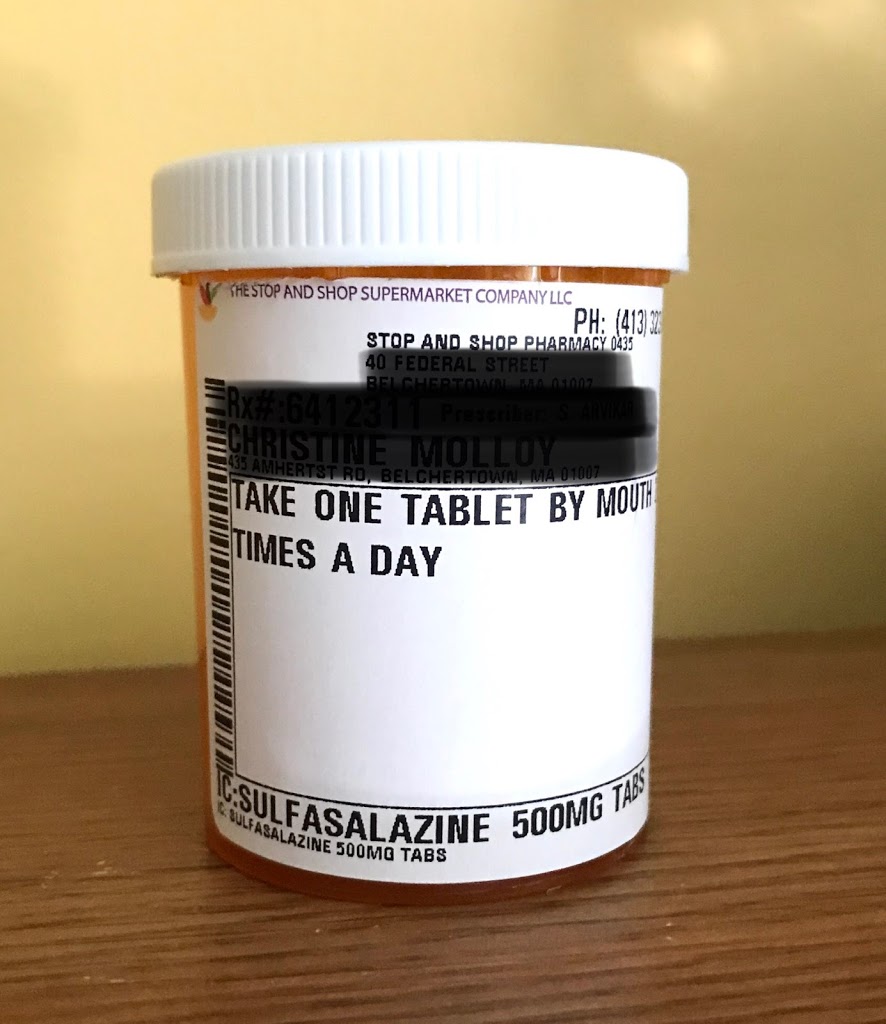
During my appointment, my rheumatologist also mentioned a medication called Sulfasalazine. It is classified as a DMARD (disease-modifying antirheumatic drug), which is also what Plaquenil is. However, it appears that they work on two different pathways and one article I stumbled upon mentioned that the two together could be more effective than either alone.
Part of the issues I have in managing my disease is that I cannot take any NSAIDs, including Motrin, Celebrex and others due to a history of gastritis (which can occur in Sjogren’s patients), and stomach ulcers, which are a consequence of the NSAIDs. I do take a medication called Tramadol from time to time for my pain, but I have been asked by my gastrointestional (GI) team to not take these medications as they can cause some GI issues and worsen others.
The part that threw me off when my doctor mentioned this medication is that nobody had ever mentioned it to me before as a possible treatment. It is often used in patients with ulcerative colitis and rheumatoid arthritis. I distinctly remember administering it to my pediatric patients with ulcerative colitis when I worked at a children’s hospital. Anyone who follows my blog, or knows me in real life, knows that I have a very extensive working knowledge of Sjogren’s. I keep up-to-date on treatments, research, all of it. I will admit though that over the past year or two, I have been working hard at trying to shift my mental focus from thinking about Sjogren’s all the time and have not kept up as much as I used to. However I thought I knew about all the medication possibilities. This goes to show you how important it is to be an informed patient.
From what my doctor said, it is not a medication that is often used for Sjogren’s. Her main concern was that it has several potential GI side effects that are exactly the same symptoms I went through hell with for two years, and finally got under control at the end of last year.
I decided I would see how the prednisone course went and meanwhile, I talked to a few Sjogren’s patients. Some of them had positive results with it, some have not, and many reported side effects. Sometimes the GI side effects are temporary and the risk can be lessened by starting the medication off slowly, meaning lower doses and at a lower frequency. Because it is a sulfa drug, there is also a risk on an allergic reaction, but I’ve taken enough sulfa drugs to not be very concerned about that.
I also decided to have a conversation with my GI team, whom I trust implicitly. They agreed with my rheumatologist about the potential GI issues, but compared to taking the NSAIDs, Celebrex, and Tramadol, they thought it was the best of all options to go with, if I could tolerate it. Of course, it’s expected I will report anything unusual that may occur.
I did my online research and read about the side effects, the blood work that needs to be periodically drawn, and the fact that it can take two to three months to see any positive benefits. The decision was made to start it now, while I’m still doing well on the prednisone, to give the medication a head start to work.
I have to be honest, I was nervous about it. I think the main reason I was nervous about it is because of the possible GI side effects AND the fact that it has been FOUR years since I have tried a new autoimmune medication. Plus, I am very sensitive to medications, supplements, all of it. I prayed about the decision quite a bit and found peace in knowing that in my decision making process, I have kept doing the next right thing…the MD discussions, the research, and talking to patients. Now, it’s all up to God and paying attention to my body.
I believe strongly that at this point in my journey, I have too much to lose to NOT try it. I have the bottle here at home with me now. It has to be taken with food, which is going to be a huge challenge since I do intermittent fasting, but for now, it’s only once a day, and that I can manage. I was going to start it today but then realized that I have to go to an appointment this afternoon and I don’t want to introduce a new medication into my system without being at home. So, tomorrow it is.
I do hope the medication helps and that I tolerate it. I have some hope, but I’m also very realistic. And if it doesn’t work, or if I have to stop it because of side effects, I’ll just keep trying to move forward.

Leave a Reply